As a young university graduate, I pursued the field of mental health and wellbeing with the intention to support others, but somewhere along the way the systems I worked in revealed themselves to be well-intentioned yet disconnected from the needs of so many coming into their care. This was especially the case for Indigenous and migrant ethnic groups.
New Zealand, along with many other countries around the globe, has been built on the back of aggressive colonisation by the British, who violently and systematically erased cultures, languages and ways of being. Jonathan Fay, psychologist and psychotherapist based in Auckland, New Zealand, describes colonisation as power and privilege meeting prejudice. The colonial ideology of domination is in stark contrast to Indigenous practices, which are founded on conservation and the connection between self and the environment. The centering of the colonial gaze and it's overarching application have undermined the value and vitality of Indigenous practices and we see this playing out politically and socially, but also in the mental health systems that are supposed to support and protect our communities.
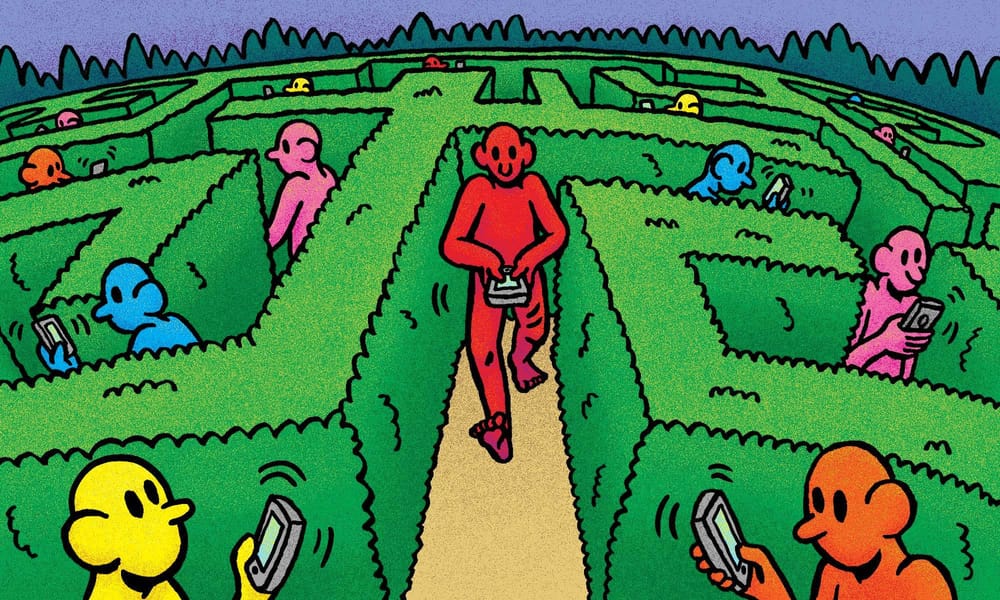
Western mental health care's focus on assessment, diagnosis and systematic categorisation has become the hegemonic way of understanding human behaviour. Colonisation crushed Indigenous forms of healing, rendering them uncivilised and unscientific which, in its wake, created a mental health system that disconnects people from their culture and communities. We see this in the form of residential centres, rehabilitation facilities, and prisons, where people are isolated from their familial environment in order to ‘heal.’ The rise of self-care culture has further perpetuated this individualistic approach to healing, which stands in stark contradiction to the collective process that BIPOC educators are advocating for, to effectively support and heal our communities on a structural level. Unfortunately, this individualistic narrative is one that many of us have come to accept, not only at an institutional level, but on a personal level too.
Western models of mental health treatment place the individual as both the source and the solution of their problems, while glossing over the systemic structures that can impact a person's wellbeing. This individualistic approach to mental health means that little recognition is given to how the experiences of discrimination, generational trauma, and compounding social factors—such as inadequate housing, food insecurity, poverty and health inequities—can degrade mental health. While treatment offered in the form of talk therapies and medication is a helpful approach for many, as a counsellor in the field with over 10 years of experience, I can tell you that six sessions of individual therapy is not enough. It will not improve the wellbeing of someone who is residing in temporary emergency housing, living on food grants, has fled from a war-torn country or whose life has been threatened because of racial violence. Their mental health is incredibly compromised by not having their basic human rights met, and refusing to address these systemic issues means that people are trapped in hopeless cycles of un-wellness for generations. Without sustainable pathways to change and strong political will, we are a society that is willing to accept and sustain systemic discrimination for those who need to be cared for the most. Not only do these issues disproportionately affect Indigenous and ethnic groups, but their very existence is the legacy of colonisation.
Mental health care in Aotearoa
In 1854 New Zealand opened its 'first 'lunatic asylum' in Karori, Wellington, to house individuals experiencing serious mental illness. It was only from the 1970's, as attitudes changed and new treatments and medication became available, that New Zealand saw a transition from institutional to more community based care. Dr Sarah Pinto, social historian, researcher and author, explains that while mental health has been deinstitutionalised in Aotearoa New Zealand, it is yet to be decolonised. We often see Indigenous populations over-represented in mental health statistics; so much so, that ethnicity alone can be considered a risk factor for mental illness. In the 2013/2014 New Zealand Health survey, it was revealed that Māori adults were 1.6 times more likely than non-Māori to experience psychological distress. If belonging to an ethnic group places you at higher risk of mental health issues, then one could argue that ethnicity is not the issue but rather a prevalence of over-diagnosis and culturally inept services that fail to understand the impact of colonisation on the wellbeing of Indigenous populations.
However, unlike other countries that have experienced the brutality of colonisation, Aotearoa New Zealand has a founding document: Te Tiriti o Waitangi, which provides a set of principles to be honoured on an institutional level. Article 2 of Te Tiriti o Waitangi is a commitment to Te Tino Rangatiratanga (self-determination), recognising that Māori authority over interventions that centre Māori are imperative. Despite this, a recent report on institutional racism in mental health found that institutional racism within mental health is pervasive in Aotearoa. Colonial violence and the historical confiscation of land, resources and culture have lead to the pathologisation of Indigenous people by Western medical models of health and wellbeing. Leading forensic psychiatrist, Dr Hinemoa Elder (Ngāti Kurī, Te Rarawa, Te Aupōuri and Ngāpuhi) states that, in reality, our health services are “illness services” whereby “people need to be moderately to severely unwell to have access to significant levels of support.” Elder elaborates on the limitations of this model, explaining how for Māori this is a life and death issue. “Māori have suffered greatly and continue to suffer because of that structure. It is not theoretical.... the individual approach is a major problem as whānau groups are affected by mental distress and illness, not only individuals.”

Training and cultural competency
Historically, many of the theories and concepts that counsellors, psychologists, psychiatrists, psychotherapists, and other mental health professionals are trained in are founded on Eurocentric ideologies, highlighting limitations in their application and effectiveness within some ethnic and racial groups. Some theorists propose universal ways of working with clients that appear to dismiss race and ethnicity—yet while there are common human experiences, these models are intrinsically flawed. No matter how empathetic a practitioner might be, good intentions do not negate the harmful impact on a client when core parts of their identity are glossed over. This dismissal of how race and ethnicity impact one’s experiences and world-views reflects a deep sense of ignorance, in a field that claims to help others.
To combat unconscious bias, there has been a rise in efforts to build cultural competency for those working within the field of mental health. Even by the 1990’s, cultural competency had become a term that was used frequently in the healthcare sector, to acknowledge that there is a ‘cultural distance’ between professionals and clients. However, this begs the question: what does it mean to be truly culturally competent? Competency alludes to the idea there is a benchmark that one can reach; however, the reality is that learning is a continuous process, an endless cycle of self-betterment.
South African university lecturer and researcher, Roy Moodley, elaborates on the importance of mental health practitioners developing cultural competency, discussing the idea of utilising Indigenous forms of healing as a means to building knowledge and developing multi-cultural therapy skills. Rather than focussing on traditional theories of mental health and responding to psychological distress, Moodley suggests exploring healing within the cultural context of the client. For example, in some cultures hearing voices or seeing things are regarded as gifts and as a possible connection to their ancestors; therefore, this is considered as something to be nurtured. However, through a Western lens that favours a primarily medical model, it could be assumed that this is a neurological disorder or reason for possible misdiagnosis. Without acknowledgement and exploration of the clients’ cultural world and the meaning they attribute to their experiences, mental health professionals may be imposing Western ideologies onto a relatively healthy client, causing further distress.
The importance of community
As social beings, community is fundamental to our wellbeing, providing us with belonging, support and connectedness. There is also a unique set of knowledge located within communities who have shared experiences; when that knowledge is valued, it can transform systems. In an interview with Rangi Davis (Ngāti-Hine, Ngāti Wai, Ngāti Manawa, Ngāpuhi-nui-tonu), a psychosynthesis practitioner and cultural advisor immersed in Te Ao Māori, she describes decolonisation more broadly as the process of “changing the colonised view of the individual to include ALL the diversity of thinking that contributes to each individual's own world views.”
Colonisation forces us to subscribe and streamline our way of being, while decolonisation fosters healing by enabling people to reclaim their ancestral knowledge. Davis explains how, in order to dismantle rigid ways of approaching mental health and provide communities with a true sense of autonomy and control, we must first acknowledge that “communities have the answers [for their own communities].” For those of us in the mental health field, that means challenging ourselves and our colleagues who are applying a one-size-fits-all model, that might be perpetuating unconscious racial bias.
At a systemic level, Indigenous populations and ethnic groups need to be trusted and supported to address the issues of their own communities, especially where racism is a contributing factor to the deterioration of wellbeing. In 2020, we saw the re-emergence of the global Black Lives Matter movement, following the death of George Floyd; an increase in racism towards Asian people, due to popular misconceptions around the origins of Covid-19; a rise in race-related complaints to the Human Rights Commission in New Zealand during the peak of the pandemic; and a terrorist attack on our Muslim community. These events are clearly rooted in racism, yet many mainstream mental health support systems are rooted in colonial hegemony. It is well researched that the therapeutic relationship is one of the primary forces of change within therapy: feeling seen, safe and understood is integral to the outcome. While empathy is certainly a fundamental quality in the therapeutic relationship, is it enough for those who have experienced racism and systemic discrimination? As both a counsellor and an ethnic minority, I would argue, no.
The pervasive undercurrent of racism and colonisation in mainstream mental health care has led to the rise of by-community-for-community services. Agencies such as Asian Family Services, Vaka Tautua, Te Rau Ora, and Sahaayta are just a few examples of service providers that deliver culturally responsive wellbeing care for their own communities. However, reliable funding and equitable access to resources are needed for cultural-community-based services to have a greater impact on their communities. Within these spaces, Indigenous and cultural systems of knowledge are used that may not be taken seriously in mainstream circles, resulting in these forms of care being identified as “alternative.” This reinforces the idea that health care, which sits outside a Eurocentric paradigm, does not hold the same value as Western practices. It is exactly this type of language that privileges Eurocentric therapies as the standard model, and sidelines anything else.

Practices such as Ayurveda, founded in India, and Romiromi, a Māori health practice, are knowledge systems that have existed for centuries, providing holistic ways of living and recognising there is more to mental health than our cognitions. Ayurveda and Romiromi both use herbal remedies, spiritual healing and physical sensations to restore balance to the mind-body-spirit, acknowledging all parts of self. When viewed through a Western lens, questions are raised about the effectiveness of these practices. When these historical knowledge systems are evaluated through medical science models built on classifications of illness, rather than concepts of care and wellness, they continue to be seen as alternative and invalid. This highlights that decolonising mental health extends beyond practice. We must also dismantle the ways we measure success and effectiveness of interventions.
The way forward
When we examine our mental health services, it is clear that many people are already contributing to meaningful structural change, but they need to be given a greater platform. As Davis points out, Indigenous and ethnic communities have their own unique set of knowledge, which has been developed over centuries, making them the best equipped to serve and support the mental health and wellbeing needs of their own people. The recent establishment of Te Aka Whai Ora (Māori Health Authority) and Te Whatu Ora (Health New Zealand) is a step in the right direction, as Elder reiterates that “Iwi Partnership Boards can potentially play a major role... our iwi members and communities are already the experts in our own solutions. When we support Indigenous and ethnic communities at an institutional and community level, there is hope for enduring systemic change.”
Any of us can work to decolonise spaces we occupy, by redistributing power and privilege. Fay explains that it is only when we thoroughly evaluate the power systems that we exist in and passively enable, that we can engage in a process whereby notions of superiority are dismantled. Decolonisation is both an individual and collective process. However, it is important to note that the intention of decolonisation is not to return to a pre-colonial state, nor is it enough to put brown faces in white spaces. Rather, it is the process of conscientising and dismantling systems that seek to dominate.
One of the most well-known holistic health models, Te Whare Tapa Wha, developed by Sir Mason Durie, has contributed significantly to understandings of holistic wellbeing. This model recognises the whole person—taha tinana (physical wellbeing), taha wairua (spiritual wellbeing), taha hinengaro (mental and emotional wellbeing) and taha whānau (connection to others).
In recognition of the important role played by whānau (extended families) in supporting Māori wellbeing and improving healing outcomes, Elder developed the intervention models Te Waka Kuaka and Te Waka Oranga, which make whānau active participants in the recovery process rather than being pushed to the periphery. This approach enables whānau to sit alongside practitioners and take a lead approach by combining the knowledge, skills and feelings of the whānau with that of the health workers, to improve both the experience of recovery and the health outcomes. While Te Waka Kuaka and Te Waka Oranga were originally developed to address traumatic brain injury, it is likely this approach will have a wider application in brain-related treatment, such as in mental health, addictions and neurodegenerative disorders. Within the addictions space, Elder has also worked alongside others to contribute to a whānau tuākana/teina model; where families that have overcome experiences with methamphetamine, are partnered with those who are still struggling. This allows for learning to be shared, breaks down isolation and possible feelings of shame, and emphasises that relationships are fundamental for rehabilitation and recovery. It is the social and familial relationships that are prioritised to create sustainable wellbeing outcomes, rather than creating dependencies on services.
Sharing indigenous perspectives in the digital mental health space is Dr Kiri Prentice (Ngāi Tūhoe and Ngāti Awa), a consultant psychiatrist and creator of Māori Minds. This educational platform is comprised of videos that highlight the value of mātauranga Māori (Māori traditional knowledge) in relation to mental health. These resources are a gift to professionals and lay people alike, fostering communication at all levels about Indigenous knowledge within clinical landscapes.
Drawing on preventative approaches to promote wellbeing with younger members of our community is the M3 Mindfulness programme, founded by Jase Te Patu, which blends Indigenous knowledge with Eastern philosophies of yoga. M3 Mindfulness utilises a Te Ao Māori-based kaupapa (principles and values) with mindfulness to engage children and youth to support mental and emotional wellbeing. Indigenous storytelling, alongside movement and breathwork, promotes emotional regulation in a format that is culturally responsive and age appropriate.
Equitable access to health care is a social justice and human rights issue, and seeking to disrupt established structures comes in many forms. Indigenous populations across the globe are advocating for change and have been paving the way forward for many years. However, the responsibility cannot and should not be theirs alone. The true decolonisation of our mental health system requires bold leadership on all fronts if we want to see a truly inclusive wellbeing approach. As individuals, that means becoming aware of our biases and reimagining mental health care as a collective process; rather than pushing others to focus on self-care only; acknowledging our duty of care to our community. If people do not feel safe seeking help from systems that were never created by them, for them or with them—and rightfully so—how can any of us expect to see the mental health of our society improving? To those of us who are non-Māori practitioners in the mental health field, Dr Elder provides us with some wise words: “Be educated. Being an ally is not enough. Have a plan to step out of the way and have Māori practitioners take your places. Know how to be a true Te Tiriti partner. Be exquisitely self-aware of the trap of centring the issues on yourselves. Listen and follow the Māori lead.”
Update: Te Aka Whai Ora, established to address the significant health disparities faced by Māori in New Zealand, was disbanded on July 1, 2024. The independent Crown entity, initially set up to give Māori a direct voice in health policies, saw its responsibilities reassigned to iwi partnership boards. This move has been met with criticism, as many fear it represents a step backward in the fight for equitable health outcomes for Māori, potentially undermining the focused and independent approach that Te Aka Whai Ora provided.