A human rights approach to healthcare puts equal rights at the centre of the design, implementation and evaluation of health systems and policies. According to the World Health Organisation (WHO) Constitution (1946), a key principle of human rights is “the right of everyone to the enjoyment of the highest attainable standard of physical and mental health.” This can be a beneficial framework, offering a universally applicable expression of the rights that benefit the individual, community and economy. Despite these guidelines, the notion of human rights can be tenuous and subjective, making them hard to implement in practice.
There are numerous barriers to realising the human right to healthcare, even in publicly funded systems like the the United Kingdom's National Health Service (NHS). While the NHS operates on a value-based approach to healthcare, where everyone is eligible for care, having the right does not necessarily mean being able to access it. As a result, the right to healthcare is not fully realised for all.
Factors that underpin the differential access to healthcare include income, employment and deprivation related to geographic location. In Northern Ireland, for example, significant increases in childhood obesity were shown to have affected deprived areas only. In this study, data was collected across 62 health indicators over time to track how they change. These indicators included things like healthy life expectancy, death rates for alcohol and prescription rates for specific drugs. Measuring such a large quantity of indicators allowed for a broad understanding of health, which was then compared over time and analysed at a regional level.
Some of the worst differential access and quality of care can be found within mental health. Although the NHS grants everyone an equal right to access mental health services, waiting list times vary significantly depending on location. This is also indicative of the lack of cohesive approaches within the NHS, which is a multifaceted service with complex issues. Some efforts have been made to address the cohesion issues with the introduction of Integrated Care Boards (ICBs), where collaborative strategies for service delivery are adopted in order to improve efficiency and access. These collaborative strategies include involving representatives from other relevant sectors to help, to encourage sharing of expertise and decision making. However, there is still a long way to go until the fragmented approach to health initiatives transforms into a fully inclusive and aligned system nationally.
A human rights approach to health in practice
The Lovepost spoke with Rajat Khosla, Director of the United Nations University International Institute of Global Health, to determine what taking a human rights approach means in practical terms. Khosla is a member of the WHO Advisory Group on Health Equity and Human Rights and previously worked at the United Nations (UN) Office of the High Commissioner for Human Rights.
Khosla believes that, ultimately, a human rights approach to health puts international human rights entitlements and claims of the ‘right-holders’ (the people, or the ‘end user’ of policies) and the obligations of the ‘duty bearer’ (the state, or the ‘creator’ of policies) at the heart of health policy plans. The key, says Khosla, is “eliminating all forms of discrimination.”
Khosla encourages global health leaders to reclaim the rights based narrative to ensure equity. This often means that we need to examine existing power structures and work to dismantle and improve them to be more equitable and fulfil their duty of incorporating human rights into all global health discussions.
There is no doubt that discriminatory policies cause and perpetuate inequality, which can have detrimental impacts on patient outcomes in healthcare. This systemic inequality is evidenced by worse health outcomes among ethnic minority groups in the United Kingdom. Action must be taken to investigate these structures and identify where discrimination can be eliminated. This is what Khosla refers to as a "bottom-up approach" to mitigating disparities. This approach focuses on root causes and strives to empower communities to take an active role in decision-making, rather than relying on top-down policies that overlook local needs and challenges. Encouraging active participation ensures that policies are suited to community needs and preferences. Ultimately, a human rights approach to health is essential for implementing such an effective bottom-up strategy, embedding core values into all levels of organisation. This could create a future where healthcare systems champion equity by prioritising the needs of all, including the most disadvantaged groups.
Khosla notes that unjust power relations are often at the forefront of development issues, and that beyond a value proposition, there is an overall failure to articulate the range of benefits that stem from adopting a human rights approach. In the United Kingdom, healthcare as a human right must be viewed beyond an ethical dimension; the economic and social benefits must also be considered. Health inequalities between the north and south of England are stark. In the north, life expectancy is up to three years shorter, and poor mental wellbeing and economic inactivity are much more prevalent. Addressing these disparities could save the economy billions, as it's potentially costing up to 5 billion GBP in reduced productivity. Moving beyond rhetoric and implementing pragmatic action is crucial to ensure that the right to health is realised in practice and that all people reap the benefits of care services.
The role of prevention in advancing health as a human right
The most sustainable solution to healthcare is to minimise the need for treatment, with preventative strategies playing a key role. Alarmingly, the United Kingdom has higher rates of preventable illnesses, such as cardiovascular disease and type 2 diabetes, compared to many European countries, underlining how a failure to invest in prevention can become a substantial barrier to healthcare access. When prevention is neglected, more people fall ill with conditions that could have been avoided, forcing an already overwhelmed healthcare system to constantly "firefight" these issues as they arise. This strain leads to longer waiting times, higher costs and worsens health inequalities, making it even harder for people to access the care they have a right to receive. As of 2023, more than 7.8 million people were on waiting lists for hospital treatment, with a growing backlog resulting from the pandemic and other factors. These delays are worsened by staff shortages and the overwhelming demand for hospital beds, which frequently operate at over 90 percent occupancy.

According to Advancing our health: prevention in the 2020s, health must be viewed “as an asset to invest in throughout our lives, and not just a problem to fix when it goes wrong." Healthcare systems in the United Kingdom currently prioritise treating existing health issues (a curative approach); however, a shift towards a more preventative approach is planned. The 2019 NHS Long Term Plan, which outlines priorities for healthcare over the next decade, includes objectives to improve access and prioritise prevention. However, in 2020, only 5 percent of NHS funding was allocated to preventative care. This reveals a significant imbalance: while treating illnesses is crucial, more investment in prevention is needed to reduce the overall burden on the healthcare system and to honour a human rights-based approach to healthcare expenditure. This is particularly important as prevention measures not only improve health but also deliver substantial economic returns, with some interventions generating a 14:1 return on investment. Successful prevention programmes, like the NHS Diabetes Prevention Programme, which led to a 7 percent decrease in new type 2 diabetes diagnoses between 2018 and 2019, demonstrate the effectiveness of such strategies.
There is also need to extend prevention beyond traditional healthcare, leveraging cost-effective methods to reduce the system's burden. For example, community programmes that cultivate social connections, which have been shown to positively impact not only mental wellbeing but also life expectancy, could be integrated. Social connection can improve a multitude of things from eating habits to sleep quality. This is a prime example of strategies outside of the healthcare system that could help to prevent the need for care later down the line. The scope for such informal care is considerable, but these interventions require local strategies to facilitate and fund non-medical support services. Monitoring the progress of these initiatives must involve a range of participants, including health economists to quantify the tangible cost of inaction as well as the benefits of preventative programmes.
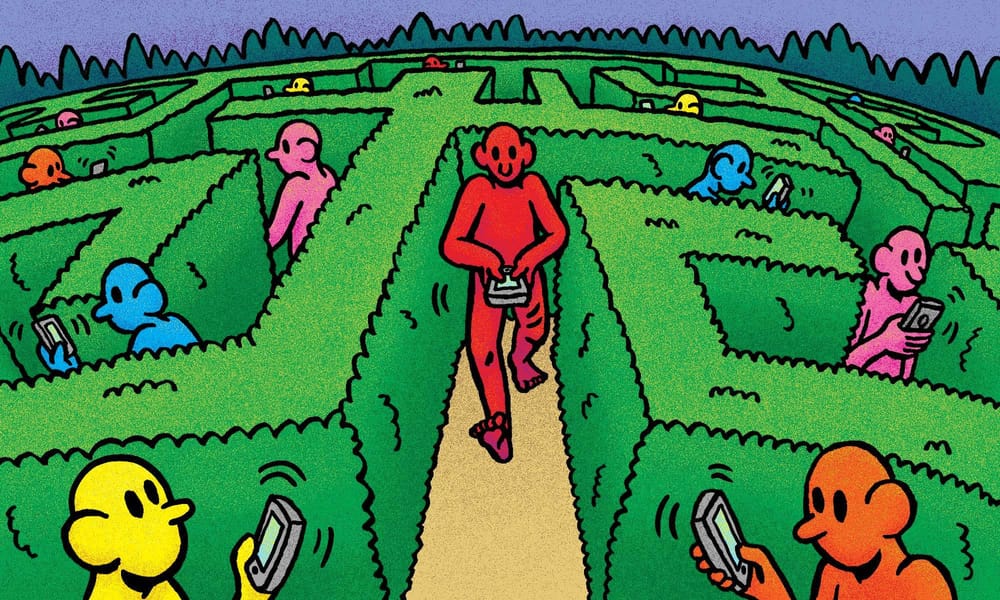
Digitisation is another tool that can facilitate secondary prevention by optimising access to healthcare. A great example is the NHS App, which is an innovative way to facilitate targeted health advice and also enables testing to help yearly diagnosis. In the United Kingdom, 33.6 million people are registered for this app. Whilst this is a fantastic advancement, a human rights-based approach to health should consider how technological advancements need be accompanied by structured digital literacy enhancement programmes to ensure that existing equity fissures are not deepened. This could include something as simple as free learning programmes to teach older generations how to navigate the app.
Resource allocation is a third area where a human rights approach can be employed. Organisational transformation is especially important in areas where there are already limited resources, and innovation adoption pathways can help to streamline these processes. Reinvesting and reorganising systems to optimise resources and money can catalyse innovation, without necessarily increasing the cost.
The data is there, but where is the political will?
Advancements in the digital monitoring of health inequalities and their precursors mean that rich data is now available and accessible like never before. Sophisticated digital tools, including real-time health dashboards, predictive analytics and AI-driven health models, provide valuable insights into disparities across regions, communities and demographics. These innovations can be used by policymakers to identify trends, predict outcomes and address the underlying social determinants of health that contribute to inequality.
However, without political willingness to act on this data, such tools are rendered ineffective. Policymakers must be committed to translating these insights into actionable strategies. This requires the political will to allocate resources, implement policies that address systemic inequities and prioritise health as a human right. Data alone is insufficient if decision-makers are unwilling to tackle the root causes of inequality—such as poverty, housing and education—or if they choose to focus solely on short-term cost-saving measures rather than long-term health investments.
"These advances have been paralleled by regressive tendencies," Khosla says. The operationalisation of health as a human right . . . has been undermined by arguments that the specificities of national contexts justify the abdication of human rights responsibilities.
"[This has resulted] in policy incoherence and an uneven implementation of international norms and standards. Furthermore, macro-level politics and ruling ideologies have been demonstrated to have a profound impact both on an individual’s realisation of their health and human rights, and on the provision of services."

The cascading repercussions of the Conservative government’s fiscal cuts to health and social care during austerity demonstrate these points. These fiscal cuts are still threatening the system, with public health grants to local authorities being cut by 26 percent per person by 2024. The high national debt was used to justify the decision to treat health as a cost instead of as a right, perpetuating barriers to funding, access and quality of care. As a result, the discrepancy between mental wellbeing in the most and least deprived areas increased between 2008 and 2013. Embracing a human rights approach to health would ensure that decision-makers prioritise human rights and funding for health and social care, instead of infringing upon them in moments of economic instability.
The varying social, economic, cultural, environmental and political factors influencing our health and care access are rightly linked to policies and laws. Health is fundamentally a political topic, thus governments need to increase their accountability for it. In an era defined by political point-scoring, it is often difficult for long-term issues such as equal access to healthcare or mobilising the prevention agenda to be prioritised in the political arena. Unfortunately, the benefits of prevention often outlive the political lifecycle and are repeatedly left at the bottom of the priority list. When combined with the rise of populism, the integration of a human rights approach to health gets continuously discarded in exchange for quick fixes.
Additionally, political volatility has a huge impact on inequality within health systems, as demonstrated by the COVID-19 pandemic, during which the mortality rate for under 65-year-olds with COVID-19 was almost four times higher in the most deprived areas compared to the least.
Khosla believes that the growing inequalities and the rising costs of treatment highlight the need for solutions that balance fairness with efficiency. He suggests that the failure to collaborate on a global scale makes it harder to tackle these challenges, especially as economic and environmental pressures increase. By focusing on human rights, Khosla says we can create more sustainable and equitable healthcare systems.
"The last decades have shown time and time again the value of human rights not only for advocacy purposes but also to provide sustained, long-term solutions," Khosla says. "Therefore, an equity-oriented approach systematically combined with human rights may help . . . address inequalities in global health more broadly."
Cooperation both within the United Kingdom, as well as globally, is a necessity to optimise resilience against threats to the right to health.
Making health a political priority
With UN political statements being criticised for lacking human rights safeguarding, it is critical to reframe health and healthcare through a human rights approach.
“First and foremost, health should be seen as a global common [good],” Khosla says. “What everyone shares on the one hand, but towards which everyone has responsibilities, on the other.”
To truly see a cultural shift in politically prioritising health, there needs to be mobilisation across industry, academia and policy making. The media, including radio and television, should harness their ability to educate and influence public opinion to cultivate a paradigm shift that champions optimal and equitable healthcare. One way that they could do this is by broadcasting personal stories of patients and healthcare professionals on television. This is an effective way to humanise the healthcare crisis and raise awareness of potential solutions.
A collaborative effort is critical to build accountability and promote a collective priority. It is essential that policies are inclusive, and through promoting patient-centred approaches, healthcare users can contribute to decision-making processes regarding their health.
Addressing the discrepancy between the ideals of rights and actual rights is critical for our future, but currently, the collaborative investment in programmes to tackle this is lacking. This is why continually engaging those who work within and outside of healthcare is paramount to embedding a culture of recentring human rights as cardinal to health.