The gift of longer lives is muted by the onset of age-related afflictions for older people. Perhaps of all these afflictions, dementia (an umbrella term for incurable, mostly late-life cognitive dysfunction, behaviour change and memory loss) is the most devastating. Its effect on a person's sense of self, relationships with others, and perceptions of the world around them is unsettling. Dementia can be profoundly stressful and confusing for the person’s family and is a condition prone to misunderstanding and misrepresentation.
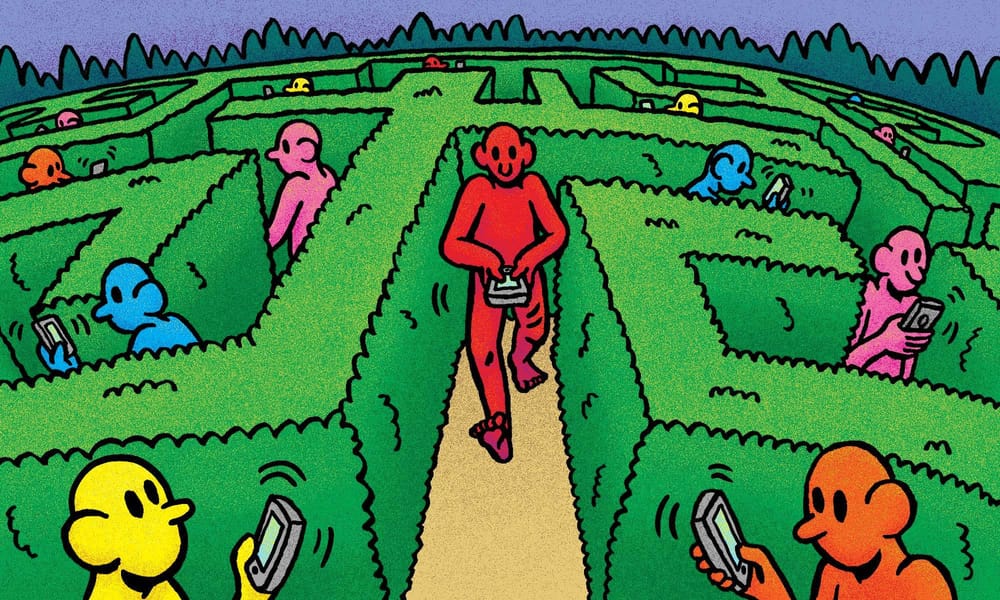
The World Health Organisation estimates that over 55 million people are currently affected. As global populations age, by 2050 this number will more than double to over 139 million. Therefore, the ways societies grapple with the prevalence of dementia and endeavour to enhance the lives of people living with dementia necessitates reexamination. With a projected shortfall of carers and concerns about inadequate human rights protections, societies need to envisage new solutions that enhance the wellbeing, rights, inclusion and needs of people living with dementia.
The Lovepost spoke to Jannette Spiering, co-founder of the world´s first ‘dementia village’ at the Hogeweyk on the outskirts of Amsterdam, to explore innovative solutions in dementia care.
Spiering is a seasoned care innovator. As a senior managing advisor for Be Advice, an advisory unit of the Vivium Care Group that owns the Hogeweyk, she helps care organisations transition to more personalised and deinstitutionalised dementia care. Three decades since the inception of the Hogeweyk pilot, numerous care organisations have embraced the vision, with similar villages popping up in New Zealand, Italy, Canada and Australia.
Over the years, the Hogeweyk has courted global interest. It has been celebrated for its person-centred approach, innovative care philosophy and better wellbeing outcomes for residents. However, the village has also been sensationalised, misrepresented and sometimes criticised.
Spiering discusses the guiding vision behind the Hogeweyk, the stifling effects of risk aversion on life-enhancing change, the power of language and some lingering misrepresentations about the village. She highlights the social responsibility we all share to improve the dignity, human rights and quality of life of people living with dementia.
What sparked the development of Hogeweyk?
In 1993, we developed the Hogeweyk care concept. At the start—and the motivation after that—was the question: how would you want to live for yourself, or for your loved ones to live their lives, if they have to move into a nursing home?
That's the question that started all this. It was, and is, still key to the development of dementia care, especially for care organisations. If you do not want to live in a care organisation that you run or design, you should rethink what you are doing.
A foundational element of your reimagining of dementia care is a concerted effort to move away from a medical care model and to normalise the everyday experiences of people with dementia. What was the reasoning behind this refocus?
We talk about rehumanising care. We advocate for, and I am an advocate of, rehumanising the care for people living with dementia. We were convinced that people with dementia are still able to experience a lot and are also able to do a lot.
When we started, we thought that creating different environments and providing care on a smaller scale that enabled people with dementia to continue to live the routine of a normal life—such as being able to participate in cooking your meals—might be very beneficial.
We knew that institutions [were] not the best form of care. We must be very honest; we created them ourselves. We thought [nursing homes] were a good step forward for people previously institutionalised in hospitals or psychiatric wards. The step to a nursing home wasn't actually bad, but it needed another step forward. We see the Hogeweyk as a very good step, but [still just] the first step away from institutionalised care.
The institutions we created were based on the medical needs of people with dementia. We treated them as patients, but we now know that you can't treat dementia. That is a very sad thing to say, but even so, we have an obligation to support them [and] to create an environment where people can go on with their lives and be supported as best we can with the things they can't do anymore. There's also an obligation to help them with the abilities they still have. That's why we wanted to move away from institutions, to get away from the medical model, and provide a social-relational model of care.

Could you unpack what you mean by a social-relational model of dementia care?
It's about putting people first and not about letting them become a diagnosis. That's the essence of it. People are social beings and need other people around them to thrive and experience quality of life. It's not enough to place them at a table . . . without anything to do during the day, [without being] able to go outside. Not living anymore but waiting there to die.
That's what we do in traditional nursing homes. I say it quite harshly now, but at the same time, I don't like to criticise existing nursing home organisations because they just function from what they know and what they think is best. It's not to say they are doing things wrong, but that we are doing things differently. [Our] criteria is entirely different from what is provided at an institute.
I've never met anyone who wants to move into an institutional nursing home. Yet last Sunday, I met someone diagnosed with dementia and on the waiting list [for] the Hogeweyk. She's alone and can't cope that long in her own home anymore. She said she can't wait to move in because she will no longer be lonely and there will be a lot of people around her. At the Hogeweyk, she has the opportunity to still be independent but also to be looked after and to socialise. She can't wait to get in. So, that’s the big difference between the Hogeweyk and an institutional nursing home, I think. Even so, it's not a situation you would wish for yourself, as dementia is the worst disease you can imagine. Still, it's different if you know the Hogeweyk and compare it to a traditional institute. Then the choice is very easy to make.
How is the vision of humanised care manifested in the physical design of the village itself? What elements do you include to create a familiar social environment for people with dementia, and how does this design contribute to the wellbeing of the residents?
You can picture the Hogeweyk as a typical neighbourhood in any small Dutch town—more urban than rural. A key element of the design is also normalcy [on a] small scale. We have 27 homes, where seven people live together and form a household.
The village includes natural wayfinding by design—different atmospheres, and different landscaping, which also helps in wayfinding. We have several amenities: restaurants, a theatre, clubrooms and a supermarket. To describe the design, well, it's nothing fancy. It's just a normal Dutch neighbourhood and the design of the houses is also very typical. You have an entrance, a large living room, a kitchen and a place where you can eat family-style, which is very beneficial for people with severe dementia. There are different dining areas, seating areas and separate places where you can still be part of the household, but also [be] more individual at a certain time of the day. You will have your own bedroom.
Small-scale design means that you can have houses with different interiors based on a person's lifestyle and what they are familiar with. We have urban interiors for those who used to live in the bigger cities, for example, or more traditional interiors in residences for more traditional Dutch people. Small-scale design allows us to work with people's lifestyles. People live together with other residents who share the same norms and values. That is so valuable. People with severe dementia benefit from recognising the people they live with, the house's interior, the meals that are cooked, the music playing, and so on. We are very aware that ‘lifestyles’ is still a kind of umbrella, or container definition, because within any lifestyle you are an individual with your own needs. But it helps.

A person's own room is also a very personal space. You can bring in your furniture and personal items. We will decorate the common spaces, but your bedroom is for you. It's your own very private space. You can do as you please in your bedroom, so there's also nothing fancy about that.
But that's why it is quite different. The normalcy is the difference compared to institutional care settings, right?
That's the difference, yes. It means that you will recognise the streets and alleys. There is a park with a pond where you can sit with other people. In front of the restaurant, we have a terrace. There is a nice fountain, and you can place your chair next to the fountain during summer, or if it's still a little bit cold, like today, you pick up your chair and you will sit with your back to the wall of the theatre where it's always warm when the sun shines. You can observe life and what's going on.
The innovation in the built environment is that we tried to make it as normal as possible because that is what people with dementia need. They need places that they understand, that they can oversee and that they can manage.
The design also creates a living environment. By placing our amenities in a certain place in the neighbourhood, we generate traffic from people who go there to do their shopping together with their carers, who go to the restaurant for a cup of coffee, or go to the cafe.

By creating traffic, you create engagement. You create the possibility of meeting other people. People are free to socialise on their own, not accompanied by a carer or anyone else. It's also a choice not to socialise if you don't feel like it—but having the sense that you are around people is important.
That's possible because at the Hogeweyk you can step out of the front door of your home unaccompanied. There's no CCTV. We will not watch you. We will not follow you because we think this is an aspect of freedom of autonomy and respect for you as an individual. All the elements that apply to you, and me as well, we also think are very, very important for people with severe dementia.
It's a choice. We know dementia villages that have CCTV. Well, if that's what makes you more comfortable, then please do. But these are our choices, which means that by giving people freedom and not locking them up as we tend to do in the traditional institute, we accept certain risks in life, such as the risk of falling.
Yes, the complexities involved in balancing a person's human rights to individual agency, self-expression, dignity, freedom from discrimination, and, at the same time, their physical safety are recurring challenges in discussions about the human rights of people with dementia. How do you balance the right of autonomy with the acceptance of risk—undoubtedly, the logic of the institutional care framework is that, “We do this for your safety.”
Yes “We keep you safe.” That's the balance that you have to make. We talk about the acceptance of calculated risk—we know there is a chance that if you walk outside, you will trip or fall, but that can also happen to me. That can happen to someone who is living on their own; an older, frail person. That can happen to everyone because risks are part of our lives.
People are sometimes very concerned about the fact that residents of the Hogeweyk walk alone and are unaccompanied, [and] that we have a fountain. “Wow,” they say, “won't people drown in your fountain?” Well, a fountain is a very regular feature of everyday life. We are more concerned that the little children visiting their granny and grandpas may fall into the fountain. If you normalise things for people with dementia, you give them the opportunity to act in a way they know. For example, our residences have knives to peel potatoes and cut vegetables and things like that. If you take that away, you take away a lot of the things that people are still able to do. Imagine that you prepared your meals for over 70 years and still like to participate in peeling potatoes. And we say, “Oh, no, that's very, very risky because you can stab your neighbour.” Well, I sometimes nick myself when I cut potatoes. That happens sometimes to residents of the Hogeweyk, but is that a risk, or is that just part of everyday life? Calculated risks are very important to discuss when you change to this model of care. Because if you don't, then you will take away a huge part of a person with dementia's quality of life.
Risk aversion is something we see in so many organisations. It's also in the government, family members and carers, everyone. It's not only the care organisation. Let's be very clear about that—it's everyone. “We want to keep our elders safe.” I've already told my children that they don't have to keep me safe if that means I will be locked in and confined to the same space for the rest of my life. It's against human rights to lock someone away, but we do it in nursing homes under the pretext of safety.
Part of my background reading highlights human rights concerns about the segregation of people with dementia from the rest of society. What are your thoughts on this?
Well, that's what we still do in the Hogeweyk. When we designed the Hogeweyk, we had to design it to keep people inside. There is one entrance that a receptionist watches, and then you enter the neighbourhood. Within the neighbourhood, people are free to go wherever they want, but they are not allowed to go outside the neighbourhood on their own. So you could say they're still locked into the neighbourhood, not in their own homes, but in the neighbourhood.
And that's part of the calculated risk you mentioned earlier?
It's also a calculated risk now to go outside. The law changed about two years ago in the Netherlands, which means that everyone—including people with severe dementia—can't be kept inside a home or an institute after a proper assessment by a multidisciplinary team at the nursing home determines they are able to go outside on their own.
We now have some residents who live in the Hogeweyk who are able to leave by themselves and find their way back independently. Together with the person's family, we decided that they could leave on their own.
But you can imagine that safety is in the minds of the family. If dad or mum can leave this neighbourhood alone, that's not why we brought them to you. We want you to keep them safe. Well, there you have the issue with safety again. If we talk about risk, the family also has to accept the risk, and then we can open our doors. However, we also have to think about the infrastructure outside. It would be very beneficial if we had quieter streets and more benches outside our neighbourhood, so people can rest after a short walk before they come back. It would also be beneficial if people in the community around us knew how to communicate with people with dementia.
I completely embrace the non-segregation of people with severe dementia and everyone with differences, but as a society, we must step up and be more inclusive. People are often fearful. “What do I do when I meet someone with dementia? How do I handle that?” If the communities around us became more aware of how to support people who have a cognitive disability, then it would become much easier.
The Hogeweyk is still a segregated neighbourhood dedicated to people with severe dementia. But it is [this way] because the outside is not yet safe for them. So, those who are against segregation, and I'm one of them, must ask ourselves a question. What are we doing so that we no longer need to segregate people?
It's too easy to point to the care organisation, because as care organisations, we are part of society, and you can't clap with one hand. If communities don't step up in their willingness to embrace people with dementia, we can't just open the doors and say to everyone, “go.” That might be too risky, and we still have a duty of care and are responsible for our residents. How can you be responsible for something that you can't influence? If care organisations can do it together with the rest of society, then it's okay.
Reflecting on my grandfather's dementia, I recall his time in an acute care facility in New Zealand during the last months of his life. He received excellent care, but he was also routinely frustrated, felt trapped and wanted to get out. How do alterations in a care facility's social and environmental conditions contribute to alleviating some of the negative experiences a person with dementia may have?
Imagine that you can't recognise where you are or that the nurses, wearing white uniforms, run around you all day and tell you what to do and when to do it. If you take away my autonomy and freedom, I will become frustrated as well.
It will only be worse if you are also diagnosed with dementia because you don't know how to cope with it. The behaviours we see are partly caused by stress, anxiety and frustration at not being able to cope with the environment, or the routines, of an organisation. Imagine you wanted to sleep in every day but must get up at 7.00 a.m. If it were me, I would not be that nice either!
So we often relate a lot of that ‘challenging behaviour’ as it is called, to the illness, but we have to be very careful because, in many instances, it is just a result of doing something that we don't want to do as a human being; we don't want to be locked in. If I lock you in for two days, you will become aggressive, and you will want to get out. And you will be angry, and maybe you will lash out. Is that because of the dementia, or is it because you feel locked in? We must be very careful.
By creating recognisable environments, such as the supermarket or a club room at the Hogeweyk, we invite people to show everyday behaviour which they have done all their lives. For example, consider if you listen to an opera in a multifunctional room with white walls, Formica table tops, and everyone sitting in a row. Maybe you haven't even chosen to be there. Your experience will be completely different compared to when you are in an environment that looks like a mini concert hall, for example, where you are only with 10 to 12 other people, where there is someone with knowledge of the subject who receives you, who knows you by name, and where you will experience a nice hour of classical music or opera. You will probably participate quite happily in an environment that triggers your brain positively. It's an environment that encourages you to show a certain behaviour. I always take myself as an example. I behave differently in a supermarket than I behave in a church or a concert hall. It's very natural. If you offer these rather specific environments to people with severe dementia, you support them in experiencing something in a positive way but also enable them to show the appropriate attitude or behaviour. We can do so much with favourable environments, as we call them.

In a favourable environment, the attitude of carers is also very important. You need to care with your hands behind your back, not take over. You need to give people time to do whatever they want to do. [It's important to] just let residents walk around in the neighbourhood and not interfere. That's also a culture change in how carers interact with people. They must be careful not to take over life but to actually support life.
Critics have suggested that the intentional construction of these favourable environments makes the Hogeweyk a bit like The Truman Show, a manipulated reality or a kind of deception. This seems a bit counterintuitive, given that part of the motivation to build Hogeweyk was to move away from the unnaturalness of institutional care. What do you make of these claims?
Well, first of all, they are made by people who have never been to the Hogeweyk, right? So I'm also always curious how you can get so opinionated about something you haven't experienced yourself because what you see at the Hogeweyk is what you get.
There's nothing staged, nothing unreal about the life inside, as it is in The Truman Show. Our waiters are not care staff dressed as waiters. Our supermarket manager is just a supermarket manager, not a carer dressed as a manager. We do not bring everything bought in our shop back to the supermarket in the evening. We do not have a bus stop, which is always said about the Hogeweyk. We don't have it. We don't fool people. Volunteers come in daily, and families come in whenever they want. Nothing is staged. Everything is real, so I think it's far away from what The Truman Show tries to be. I don't actually understand the comparison, and I think it's damaging to what we are doing.
Misrepresentations can fuel misunderstandings, no more so than in the language we use. Why is language important when discussing people with severe cognitive difficulties? Your website notes a bit of scepticism about the term ‘dementia villages’, for example.
Well, we now carry it like a kind of compliment, but we were dubbed a ‘dementia village’ by CNN [Cable News Network]. CNN came to make a documentary in 2013, and because they couldn't pronounce Hogeweyk, they called it a ‘dementia village’ as it's so much easier to pronounce.
It describes what it is: a village for people with severe dementia. We wanted to get away from the institutions that are stigmatising. Now we've got another name, which can also be very stigmatising because it suggests we created a special or different environment. So that's why we are not that happy with it. But on the other hand, it makes clear what it is and makes people understand what we are doing. Often, when we talk about people with dementia, it's about ‘us’ and ‘them’. It is as if they are another species. And in that way, it contributes to the dehumanisation of people with dementia.
If you read institutional language it often talks about ‘allowing’ people to do certain things while they live in a nursing home. It would be much better to say that people can and have the right to do certain things if they want, just like you and me. Language is a very strong driver of change. The words we use in institutions are not those we would use when we talk about our daily lives. So, if you keep talking about ‘food intake’ for people instead of just meal time, or if you keep talking about therapy—music therapy, pet therapy, or aromatherapy—for people with severe dementia, you make it as if they are living in a world separate from us.
If I go to a concert, I don't return home and say to my husband, “I've had great music therapy this evening!” No, I can only tell him if it was good for me or not. It might have a therapeutic effect on me, but it's not therapy. If you medicalise things and use medical words, you remove the normalcy that we want to create. And the more normal the language is, the better it is at driving the change. People speak about ‘wanderers’. I take a short walk through the neighbourhood every day. I do this because it's bad for me to sit on my butt all day. Am I a ‘wanderer’ or am I just someone walking around? People with dementia go outside because they want to enjoy the fresh air, not because they are all ‘wanderers’.
A challenge to the widespread adoption of the social care model for people living with dementia appears linked to a perceived limited evidence base. Research on the Hogeweyk does point to the reduction in the use of pacifying medications and anxiety symptoms. Still, others believe more evidence is needed. I point here to Boston University public health policy analyst Kristina Carvalho, who writes that we just don't know if dementia villages work. How would you respond to this?
What we do know is that traditional institutions don't make us happy or enhance quality of life. So I always become a little bit annoyed about [comments like this], because if you are not willing to accept new outcomes without extensive research, nothing will change. You have to innovate to see what will come out, but by just theoretically approaching a subject like this, well, you will get quotes like that: “We just don't know!” But if you don't try, you will never know the effect. The effects of our pilot 30 years ago were very, very encouraging.
By creating smaller group homes instead of wards, we were able to cook together, we were able to develop a normal household for people. The environment immediately encouraged more rest, less anxious behaviour and more engagement in the daily routines of life. We experimented with all these elements and others, such as the culture change in how the staff related to residents, and found out what would be best for the residents. We discovered that this new way did increase their quality of life. We gave ourselves one year for the pilot . . . with thirty residents. However, within the year, the whole organisation shifted because the results were so positive, not only for residents, but also for carers. It gave carers back their professional autonomy. Carers were no longer following the organisation's routines but following residents' lives and rhythms. If I quote those who visit the Hogeweyk, or other organisations who followed in our footsteps, they will see residents who are more independent and look less anxious. Of course, some of the residents show behaviours we still do not understand but much less so than in traditional care.
Nourishment is not an issue with us because we have family-style dining, eating together in normal terms, which ensures that you eat better because you have time to eat and socialise. It's a normal process. Instead of being served something that you do not have any clue where it comes from and don't have enough time to eat because the dishes have to be rolled back to the central kitchen.
At the Hogeweyk, people look well cared for. If we walk around with groups of visitors, residents love to connect with visitors because they are curious about who these people are. A normal environment creates normalcy, and people blend in. Sometimes you can't even recognise who [are] the residents. Maybe we don't know how it works like this, but we know it works. We know that it's completely different with many positive outcomes. Over the last 30 years, so many elements of what we do have been researched that we dare to [refer to] an evidence-informed model—not evidence-based but evidence-informed.

The example I gave about family-style dining—it has been researched, I think now, more than 15 or 16 times, over and over. It's not too difficult to find out that you feel more comfortable in your home with only six or seven people around you, rather than in a ward with thirty others, where everyone's running around and making lots of noises, and you are sitting there with your affected and damaged brain not being able to cope with all that. But it has been researched and has benefited residents, so we are very happy.
Yes, my understanding is that the efficacy of the social model of care is quite well established for many other mental and physical health conditions, especially the role of social connection and social groupings to alleviate loneliness and isolation. Is the issue that it's not especially targeted to people living with dementia?
I know that research is necessary to prove change and to prove that one thing might be better than something else. But what always puzzles me is that researchers—no, all of us— look at people diagnosed with dementia as being different to us ourselves. Everything is related to the dementia, but people with dementia still have the same needs as me and you. They are just normal human beings. If it's cold, they will shiver. Let's not make it too complicated. The question should be: how can we change the systems around them in order to support what's still there? Of course, we have to research and understand the affected brain and behaviour changes. It's difficult to find out what makes people tick or what causes aggression.
We have dementia coaches in the Hogeweyk who are highly trained in observing that challenging behaviour and trying to find a way to cope with it, and sometimes we can't cope with it. We must also be very honest about that. For maybe 20 percent of those diagnosed with dementia, we can't come up with a solution to improve their quality of life as a whole. But for the other 80 percent, we can do a lot with this new approach to care.
A question at the back of my mind is whether or not the Hogeweyk is an example of Dutch exceptionalism. It was primarily funded through the Dutch social insurance fund, which provides significantly higher public funding than many other countries. True, despite its innovations, the per-person cost to the public wallet is similar to that at a regular nursing home. But in countries with lower public funding, how has this reality resulted in different realisations of the Hogeweyk Care vision? Does the vision change when confronted with local realities?
When organisations or other groups visit us, we always say, “Don't copy us.” You have to accommodate the country you're in, its norms and values, the architecture, the health system, and the finances.
So that means . . . that there are different outcomes in how the other dementia villages are constructed or run. There are various group sizes because it's better to have eight or even 12 people within a certain budget. In Canada, they have Langley Village, which has groups of 12. If that is what makes it possible, then we will never judge it. It's about looking at the possibilities in that regard. However we see that our care model, our way of thinking, can be replicated everywhere. Yes, we see differences in terms of group size, the number of homes, whether you have a vibrant club life like we have or not, whether you can have a full-functioning supermarket or not, whether you can cook in the homes or not, or just maybe finish [the meal] off when it is delivered to you. All places have different outcomes, but the philosophy of normalcy, respect for the autonomy and dignity of people, and providing choice and freedom—those values we see everywhere.
There are also different outcomes in how we see it being implemented in for-profit and not-for-profit care organisations. Sometimes, for-profit organisations can take the initiative because they have money and can experiment more. They can lead the way for the not-for-profit ones because the for-profit ones have to stick to the same rules and regulations. So, a lot comes down to a change in attitude and culture. Of course, it's nice to have nice environments and nice buildings. You can compare the for-profit micro-town near Brisbane, and the not-for-profit village in Rotorua. The micro-town might have had a larger budget to spend on the built environment than the one near Rotorua, but both have the same philosophy of care. They work with lifestyles and they work on a small scale.
What's involved in changing the culture of care organisations to a more humane model?
There is so much to it because if you change to another model of care, then it involves a paradigm shift. It's a shift in the organisation, a shift in design, a shift in vision. Culture change takes quite some time. If you try to convince people that working in a different way is best for them and others, that won't work. If you give them room to experiment and feel for themselves what it means for them and the effects it creates for others, then they will step forward.
So, there is also an issue of change management and how to do that. It took us quite some time, but what helped us, and is [part of] why we succeeded, is that we created a very easy vision to transmit to [those we made] this change with. It's for everyone, it's easy to understand, and we stuck to it.
We also never wavered from our principles of normalcy. If something needed development, we always asked ourselves a question. Is it normal, or is it institutional? Is this something you would like for yourself or your parents? If it's an answer to a protocol or something we must do due to policy, then we really have to think about it. If we can't escape from policy or regulation, how can we do it in a way that will fit our vision? You can do a lot within the existing rules and regulations while still sticking to your vision. There are also things that you can't change. So, you need to choose your battles and go on with what you can influence and what you can change. That's how our development went.
I think that culture change requires a strong vision and a very dedicated team that has been in place for quite a long time. Look at myself: I started working here more than 40 years ago and am still here. So, consistency in the team, its vision, and how they want to progress with the development of the innovation.
Finally, what do you hope the future of care for older people will look like, or what would you like to see it look like?
If society were more willing to embrace those who are different, we would not have to segregate so many different groups of people. [With] more knowledge in society about dementia and how to support someone in their home environment, people can live longer at home. And that will be necessary in the near future because of the large number of people who will grow old, many of [whom] will unfortunately be diagnosed with dementia.
It is an unfeasible task to build more and more nursing homes or dementia villages, because we simply cannot find enough staff. The Hogeweyk is a great example of what deinstitutionalisation can bring to traditional nursing home care, but also to a social approach to people with dementia at home. We have to change the system that we created ourselves. We will have to embrace a life with risk, and [accept] that we can't keep everyone safe.
Deinstitutionalising, transforming, and normalising everything in healthcare might help create a better future for everyone. There is a whole movement of change going on around the world. We are part of that. We drive that with our care and support for other organisations. But we also have to consider that it's a huge paradigm shift. It will take pioneers . . . to prove that this is also a better way than the institutionalised way we know now, which no one wants to live in.
So, I think our step away from the institute shows that it can be done and that it can be replicated all around the world. The outcomes of how people experience quality of life are the same worldwide. People are happier, need less medication and feel better. We do not know if they live longer, or [whether] they live less long due to all the risks from falling incidents, but then you might have had a nice life for the last two and a half years . . . instead of being locked in and dying of boredom.
It's a shared responsibility to open people's minds to the fact that things really can be done differently. That dementia, although scary, can also be supported better, and that we can also create some happiness in people's lives.